If you had asked two months ago how my heart health was I would have laughed at the absurdity of the question. Why ask about something so obvious? My heartrate was consistently around fifty—a runner’s heart. It took a herculean effort to get it above 140, and then it came down precipitously fast as soon as I stopped whatever I was doing. I never had symptoms of anything heart related. In fact, I climbed Mt. St. Helens a year earlier. Although it taxed me like nothing before, I made it up and down and recovered quickly.
In response to the question, I would have said I had a healthy heart. In fact, my heart would have been the least of my nascent post-sixty health issues. Bad knees, sore hips, hernia, skin biopsies, sleep apnea were the beginning of what I still hoped would be a long joyful march to the grave. I was adjusting to whatever arose and looking ahead to the next big challenge. Should I hike the Appalachian Trail or part of it? Should I go on a long, multi-day bike trek? Should I raise my level of swimming, with the goal of swimming in Lake Michigan every day? It all seemed possible, and with retirement three years away, I figured I’d have the time to do any or all of these and more.
But, things changed, and the heart question would have been prescient.
At the end of my annual physical in August, my doctor asked me if I wanted a heart scan. “Only $49,” he said. “Insurance doesn’t cover it, but hey for forty-nine bucks, it’s worth doing even if you don’t need it.”
I didn’t need it, but hubris said do it. It would be proof of how fit I am. I did it.
The scan results showed up a week later in my medical portal. I copied and pasted medical terminology into Google to understand what they meant. One of four arteries was seriously obstructed—calcium buildup—so much so I was categorized as having a 77% greater chance of having a heart attack by age 70 than people my age.
Wait! Seriously, I thought. People who don’t exercise? Who drink and smoke? Who are overweight? Have a better heart than me?
My doctor wasn’t concerned…yet. The test is new, he said. Who’s to say how accurate it is. He referred me for a stress test.
I wasn’t worried. Again, hubris said I’d show them. Put me on a treadmill, and I’ll go all day.
Two weeks later I got on the treadmill, wire regalia in place, and told to go. I did, through part 1….part 2….part 3 of three parts. I hit a 140 heartrate, a few percentage points above the sought after 85% of heart exertion. I was moving, and then I was done. The technician said let’s stop there. I’d completed the test. My blood pressure had risen as expected and recovered quickly. There was no pain and no aftereffects. EKG was good.
With the result spewing out of the machine, the technician went from sounding like a distant, only-the-cold-hard-facts scientist to a concerned mother. She said I should hear from my doctor in a day or two. Check the portal, every day, she said, her expression saying she meant it.
It was the weekend. The results hit the portal before I heard from my doctor. I copied and pasted again. It wasn’t good. When it reached 142 bpm, my heart wasn’t getting enough oxygen. The blood flow was severely blocked. Although I wasn’t physically experiencing pain or even discomfort, my heart was struggling. It just didn’t want to tell the rest of my body.
I messaged my doctor: “At what point should I be taking this seriously?” I asked.
He didn’t text me back. On Monday, he called and left a message. “I want you to go see a cardiologist and get an angiogram,” he said. He gave me a name and phone number and said call now.
I called and got an appointment for two months later. That seemed far off, so I messaged my doctor and told him I had changed insurances recently, so had more options.
My doctor immediately messaged me the name of another cardiologist in a different hospital. I got an appointment within a week.
Here’s the kicker in all this, or the feather that broke the camel’s back. About the time I had the stress test and a couple weeks before I was to see the cardiologist, I started having discomfort in my chest (yes, really!). Nothing painful. Nothing that affected my routine. It neither got worse with exercise nor better with rest. It was there, a dull heaviness, constantly, an annoyance in my chest, never moving elsewhere in my body.
Hubris had left the building, and paranoia had taken up residence. I was making shit up, I told myself. It was in my head. I didn’t tell anyone, but I did keep track of it. I would tell the cardiologist and let him tell me I was crazy.
I took the scan and stress test results to the cardiologist (different medical network, remember) and told the nurse taking my vitals about my chest pain. She typed away like I was the lead character in the novel she was writing. She did a quick EKG, pronounced it fine, and told me to sit tight. The doctor would be in momentarily.
Fifteen minutes later in he came, all business. He was an unassuming, soft spoken, balding man a few years older than me. He introduced himself, holding the handshake for longer than I expected. He told me to sit down. He pulled his chair on wheels over to me and sat facing me, two feet away. “It's good to meet you,” he said. “I’ve looked at your tests…and the intake notes and, although I don’t know you….and you don’t know me, I want to tell you something. You can do what you think is best. Based on what I know, though, I think you need to go to the hospital right now.”
“You mean from here?” I asked.
“Yes, from here. We will call an ambulance.”
Within ten minutes, Chicago firemen and paramedics were in the exam room and along the hall. That’s Chicago. Need an ambulance, and they’ll throw in a firetruck to clear the way.
They looked me up and down, seemingly disappointed I was nothing more than a 64-year-old sitting comfortably in an exam room. Still, they had to wheel me out in a medical chair. Protocol.
In the medical van, a paramedic hooked me to an IV while talking with another paramedic about the promotion exam he was thinking about taking. “What’s wrong with him?” the driver asked, nodding at me.
“Heart trauma,” the paramedic said. “How do you feel?” he asked me.
“Fine,” I said.
“Heart attack?” the other paramedic asked, as he climbed in beside me.
“Not yet,” the one standing over me said. He called ahead to the hospital. “Cardio trauma two minutes out,” he said.
Sirens blasting, I rode the two blocks to the hospital. It took ten seconds. They wheeled me into the ER past all those waiting and into an empty exam room.
Seeing me, a nurse asked, “This is the cardio trauma?” The paramedics and I nodded, and she went to work. Within ten minutes, I was hooked up to EKG wires and being fed blood thinner through my IV. At this point, they were determined not to let me have a heart attack.
Over the next two days, the hospital intercom would blast, “Cardio trauma incoming,” or something like that every few hours, signaling the arrival of a heart attack victim or someone like me, a lucky person with diagnosed heart disease yet to turn into full fledge trauma.
I imagine the same call going out across the airwaves immediately after the paramedics called in to say I was coming. Hearing it brought home the seriousness of what was happening. Hubris or ignorance had done a job on me for many years. The whole experience was a reckoning and each incoming trauma call a reminder.
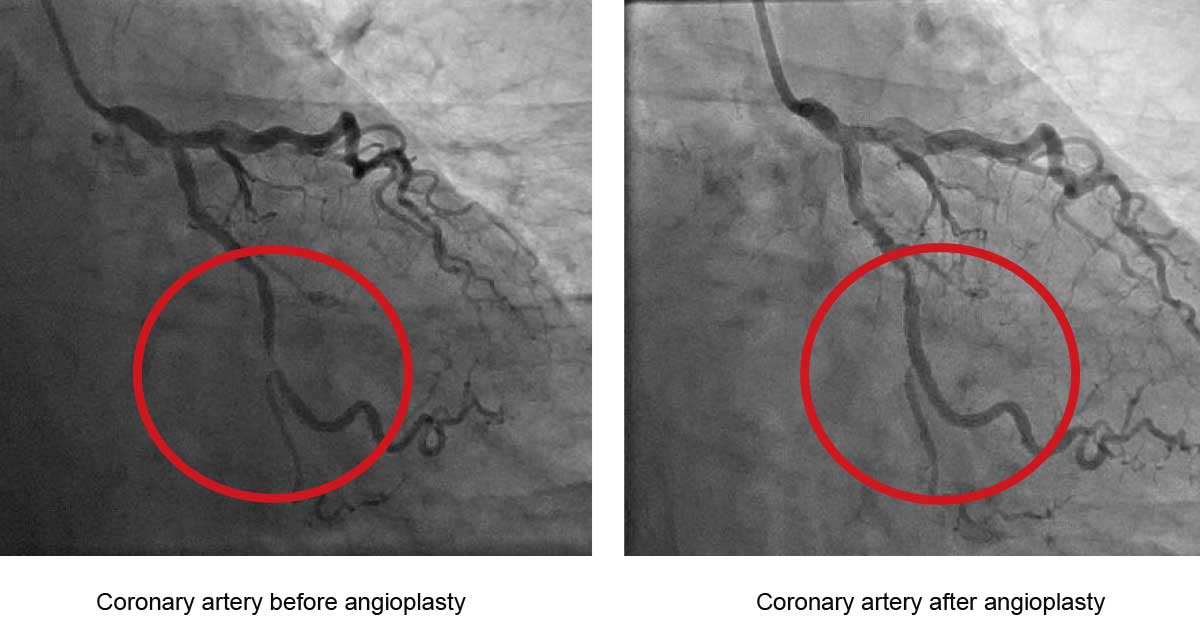
The next day I was second in the queue for an angiogram, followed by an angioplasty. In at 10:30, out by noon, I couldn’t move any part of my body except my head and left arm for four hours after. The artery in question was 80% obstructed, worthy of one stent.
I went home the next day, artery opened, chest discomfort gone, wrist and groin incision points seriously bruised but remarkably healed over.
I no longer saw living past ninety-nine as inevitable. I’m fine with that. In fact, I’m better than fine. I’m lucky.